Is Malignant Hyperthermia preventable?
Share this article:
Click the image to visit the Pentland Medical website (UK distributor).
Malignant hyperthermia (MH) can kill. Unfortunately, unless you know that your patient is at risk, MH tends to present as an anaesthetic emergency.
MH is an inherited disorder; the ryanodine receptor in skeletal muscle is abnormal and interferes with the regulation of calcium in the muscle. The resulting build-up of calcium is a massive metabolic reaction [1]. It presents as a clinical syndrome of hyper-metabolism involving the skeletal muscle, triggered in susceptible individuals primarily by anaesthetic agents and the muscle relaxant succinylcholine. The signs of MH include muscle rigidity, rapid heart rate, high body temperature, muscle breakdown and increased acid content.
Vapor-Clean Activated Charcoal Filters
Because newer anaesthesia gas machines contain plastic and elastomeric components that both absorb volatile anaesthetics and release residual vapour during subsequent anaesthetic procedures, purging using high flow for a long period is required. Table 1 indicates flushing times.
Table 1: Anaesthetic machine flushing times (to inspired agent <5ppm)
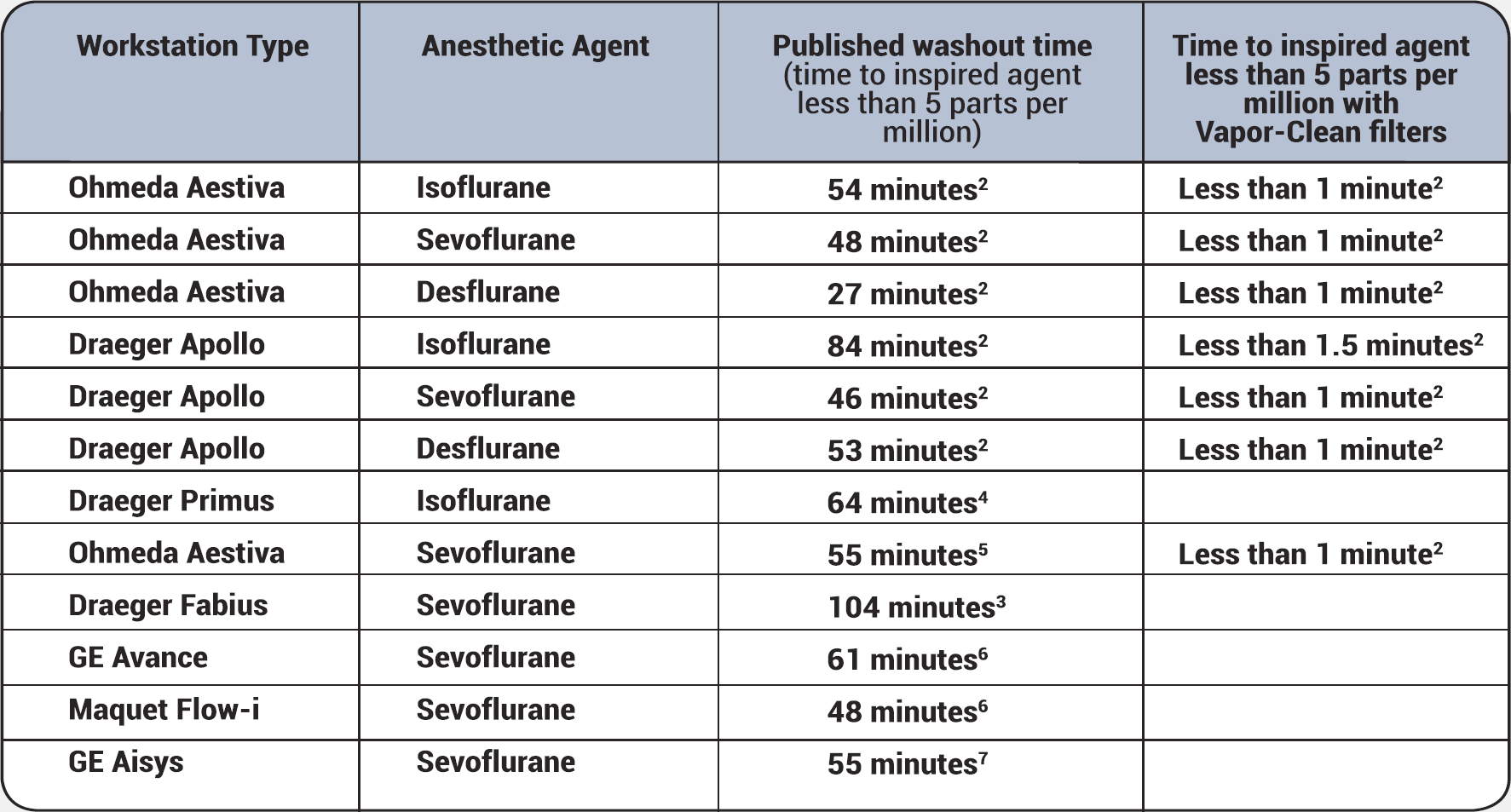
Vapor-Clean activated charcoal filters (Dynasthetics, US, distributed by Pentland Medical UK) negate the need for lengthy flushing; in less than 90 seconds, they absorb any trace amounts of isoflurane, sevoflurane and desflurane so that anaesthetic vapours do not reach the patient.
The Vapor-Clean charcoal filters are designed to be placed between the anaesthesia machine and the inspiratory and expiratory limbs of the breathing circuit. The concentration of anaesthetic vapour that protects the susceptible patient from an MH reaction has never been determined with certainty, but concentrations less than 5ppm are generally considered acceptable; Vapor-Clean filters exceed that goal.
In addition:
- They are compatible with all anaesthesia machines
- They have a two-year minimum shelf-life
- Avoiding a ‘surprise’ MH patient means that costly operating room delays are reduced
- They present negligible additional circuit breathing resistance
- There is no need to remove the C02 absorbant when using them
Avoiding MH
Unless you know that your patient is susceptible to MH, it is impossible to tell which patient may succumb. Therefore, prevention is essential. The Malignant Hyperthermia Association of the United States (MHAUS) [2] suggests that every anaesthetic should have a plan for treatment of unanticipated MH. In addition, MHAUS evaluated the use Vapor-Clean activated charcoal filters to minimise residual exposure, and recommended them for use, stating:
For both new and older machines, adding commercially available activated charcoal filters to the circuit will remove anesthetic gases and obviate the need for purging the system…. However, the anesthesia machine will still need to be flushed with high fresh gas flows (≥10L/min) for 90 seconds prior to placing the activated charcoal filters on both the inspiratory and expiratory ports. These filters are effective in keeping gas concentration below 5ppm for up to 12 hours with fresh gas flows of at least 3L/min. [2]
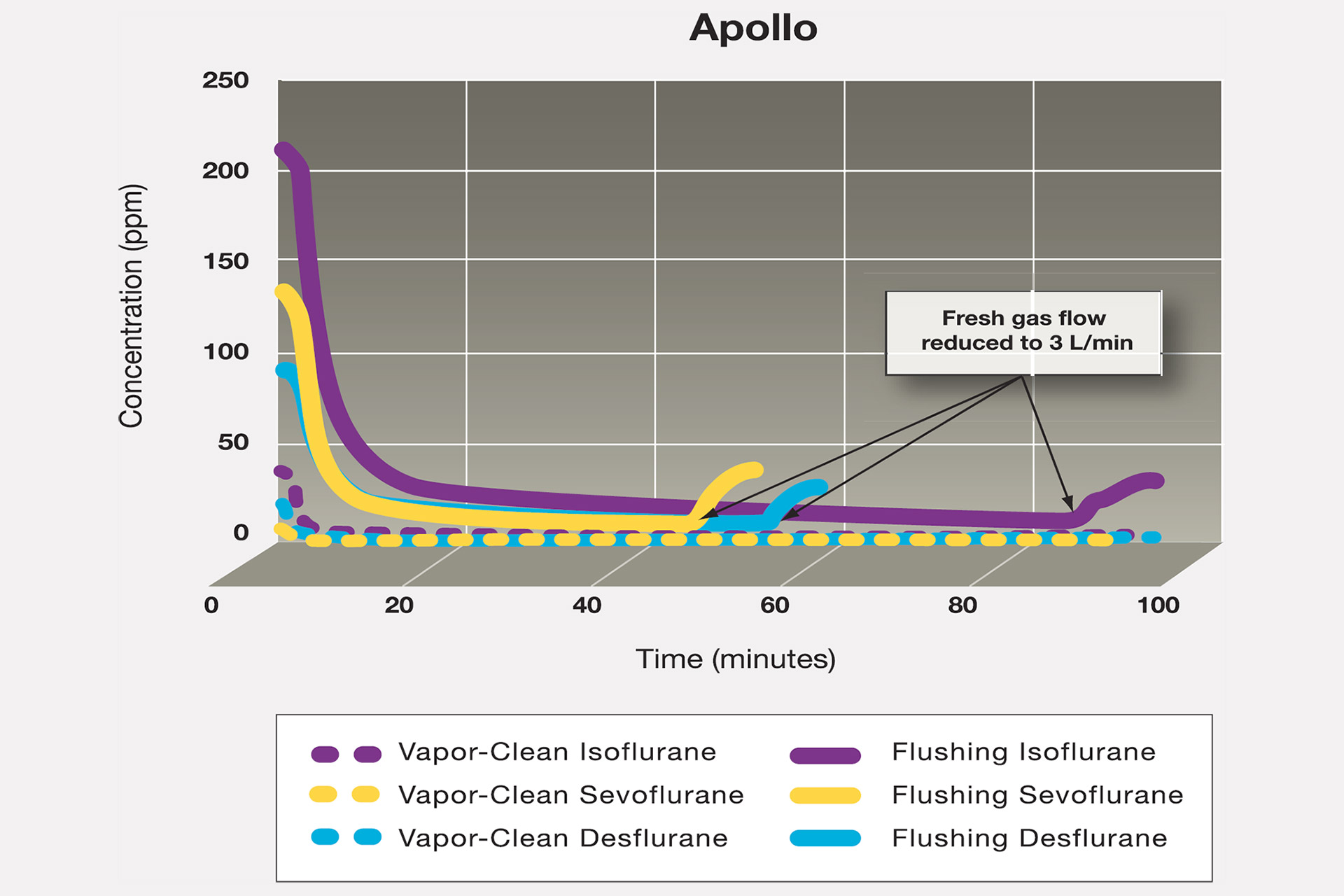
Birgenheier et al’s study [3] determined anaesthetic machine preparation time both with and without Vapor-Clean filters. Results showed that without the activated charcoal filters, it took 78 min and 55 minutes for the inspired isoflurane concentrations fall below 5ppm in the Apollo and Aestiva machines respectively. With the activated charcoal filters, the inspired isoflurane concentration was immediately less than 5ppm and remained below 0.63ppm for 45 min in the Apollo machine and below 0.39ppm in the Aestiva. Figure 1 shows the comparison using the Apollo machine. The authors concluded that activated charcoal filters provide an effective way to prepare modern anaesthesia machines for MH-susceptible patients, that no flush was needed for the machines, and inspired agent concentrations were < 5ppm, independent of fresh gas flow.
Figure 1: Flushing times using activated charcoal
Similar results were noted by Stoker et al [4]. Feldman [5] (suggests that:
“With the advent of the Vapor-Clean device, it would seem that the challenge of protecting MH susceptible patients from trace amounts of anesthetic vapor has been solved.”
In the event of a MH crisis, the anaesthetic gas can be quickly turned off and Vapor-Clean filters inserted to curtail further exposure without delaying the administration of dantrolene and without the need for manual ventilation.
Conclusion
Vapor-Clean filters have been shown to reduce residual anaesthetic gases for up to 12 hours. In addition, they reduce the need for lengthy flushing of anaesthetic machines prior to using on another patient. This represents both a resource saving and a potential life saving measure in both known and unknown MH risk patients.
If you would like to comment on any of the issues raised by this article, particularly from your own experience or insight, Healthcare-Arena would welcome your views.
References
- Chapin JW. Malignant Hyperthermia. Medscape. 2014. http://emedicine.medscape.com/article/2231150-overview Accessed August 2015
- MHAUS. Preparing the Anesthesia Machine for MHS Patients. 2015. http://www.mhaus.org/healthcare-professionals/be-prepared/preparing-the-anesthesia-machine Accessed August 2015
- Birgenheier NM, Westenskow DR, Orr JA. Using Activated Charcoal Filters To Prepare Newer Anesthesia Machines for MH-Susceptible Patients. Poster presentation. ASA. 2009. Abstract available at: http://www.dynasthetics.com/Vapor-Clean/study-uofu.html Accessed August 2015
- Stoker R, Romankowski M, Burk KM, Orr JA. 2 Hour Evaluation of Filters to Prepare an Anesthesia Machine for Malignant Hyperthermia Susceptible Patients. Poster presentation. ASA. 2011. Abstract available at: http://www.abstractsonline.com/plan/ViewAbstract.aspx?mID=3194&sKey=e6a9a3d0-3035-4aa4-b921-047d333fb478&cKey=c2ec5847-ec0d-41b0-ae72-9dbf1fe28344&mKey=6423fac7-aec2-4629-97e9-148ef95e3184# Accessed August 2015
- Feldman JM. New Device Simplifies Workstation Preparation for Malignant Hyperthermia-susceptible Patients. Anesthesiology. 2011. 8; 115: 434. http://anesthesiology.pubs.asahq.org/article.aspx?articleid=1933856&resultClick=1 Accessed August 2015













Comments are moderated and may not appear on the site immediately.